A new development in a Georgetown lab could revolutionize the treatment for patients with late-stage multiple sclerosis and slow the progression of the disease.
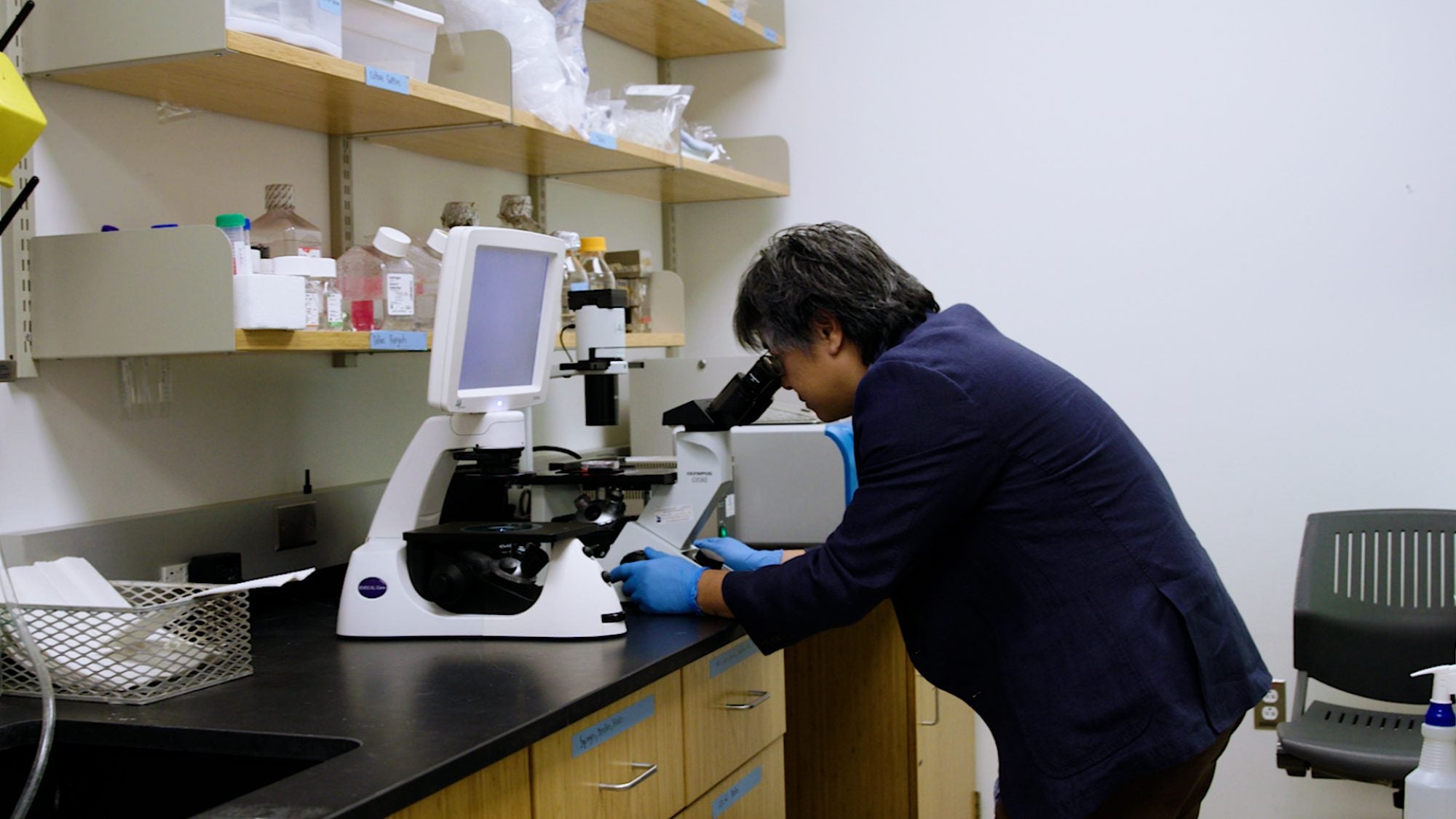
Jeffrey Huang, a provost’s distinguished associate professor in the College of Arts & Sciences’ Department of Biology, and his team have developed a novel drug application that reversed the effects of late-stage MS in mice. The drug is now being planned for a clinical trial on people with MS.
“Our team is ecstatic to move to clinical trials,” said Huang, who is also the deputy director of the Center for Cell Reprogramming. “Based on our success in animal trials, we believe our drug will help stabilize patients with the disease, reducing not only the number of relapses, but their severity as well.”
The Mechanics of Multiple Sclerosis
Multiple sclerosis, often abbreviated to MS, is an autoimmune disease that affects some 2.8 million people worldwide. MS causes the body to attack the protective coverings that surround nerve cells in the brain, called myelin.
“Myelin is like the insulation around copper wires, which are your nerves,” explained Huang. “In order for nerve cells to communicate, they rely on myelin. If there’s any damage to that insulation then that high-speed communication is severely impaired.”
As inflammation destroys myelin in the brain and spine and interrupts nerve-cell communication, patients can experience a litany of adverse health effects, including muscle spasms, loss of balance and ambulatory dysfunction. Typically, when myelin is damaged, the body is able to regenerate that protective layer fairly quickly.
“In the initial stages of MS, the body is still able to remyelinate after a flare-up, but those natural repair systems stop functioning as effectively after someone has been living with MS for a significant amount of time,” said Huang.
This new approach is distinct from available therapies for patients with MS. Current drugs on the market target the immune cells in the blood, primarily B cells and T cells, rather than those in the brain. And those drugs drop in efficiency as the disease progresses. Huang is applying an existing drug to MG for the first time, which he believes will be a game changer.
A Novel Therapy for Myelin Regeneration
Huang’s approach to myelin regeneration begins by looking at the root mechanics of remyelination. That process starts with the resident immune cells in the brain and spine called microglia. Microglia are like an all-star pit crew for the brain: They clean up damage after it occurs and ensure the brain is ready to keep racing. In late-stage MS, microglia become inflamed and aggressive and have trouble communicating with the cells that spur remyelination.
“Following injury, these cells go from Bruce Banner to The Incredible Hulk, and continue to cause damage to myelin and nerve fibers in the brain and spinal cord,” said Huang. “Our drug is able to reverse its phenotype back into Bruce Banner, who can return to doing nice things in the brain.”
Huang and his team’s revolutionary method turns microglia back into its healthy, homeostatic state – and it’s already seen success.
They successfully achieved remyelination in animals such as mice by stimulating the microglia, which then starts a chain reaction in the brain and spinal cord that MS impedes. For people with late-state MS, then, this drug could revolutionize their treatment, giving patients more healthy years with increased independence.
The next steps are clinical trials in humans, which will be conducted by a pharmaceutical company working alongside the Huang team. In addition to the Huang lab, Georgetown is also home to the Center for Brain Plasticity and Recovery and Center for Neural Injury and Recovery, which studies neural plasticity, injury and recovery.
“The goal is to be able to stop the disease from progressing using our drug,” said Huang.