On August 14, the World Health Organization (WHO) declared mpox a global public health emergency of international concern after cases have sharply risen in the Democratic Republic of the Congo (DRC) and a handful of neighboring African countries.

This follows the outbreak of a different strain of mpox in 2022, when the WHO declared the disease, formerly known as monkeypox, a public health emergency.
“Mpox is an infectious disease that can cause painful rash, blisters, aches and fever, as well as swollen lymph nodes,” said Rebecca Katz, professor in the School of Medicine and School of Foreign Service and an expert in pandemic preparedness and health diplomacy. “The virus has caused occasional outbreaks in parts of Central, East and West Africa for decades, and epidemiologists have tracked thousands of cases a year in mostly Central Africa for the last 20 years.”
Katz, who is the director of the Center for Global Health Science and Security and senior advisor to Ambassador John Nkengasong at the Bureau of Global Health Security and Diplomacy in the Department of State, said that while the risk of mpox spreading widely in the U.S. is low, people need to exercise caution and vigilance. In 2021-2022, Katz also worked at the Department of State as a senior advisor on global health security and the COVID-19 response. Today, experts from the O’Neill Institute for National and Global Health Law published an opinion piece in the New York Times on the pandemic potential of mpox.
Learn more about mpox from Katz as she explains the disease’s risk factor and the lessons from the COVID-19 pandemic that can be applied to this global health emergency.
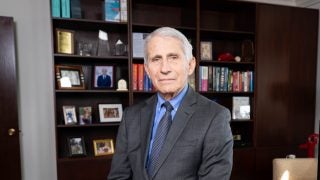
Ask a Professor: Rebecca Katz on the Risk of Mpox and Containment Strategies
What is mpox, and why did the WHO declare a global health emergency?
In July 2022, the WHO declared mpox a public health emergency of international concern after the virus spread rapidly to Europe, the Americas and eventually to 110 countries, primarily transmitting sexually to men who have sex with men. This outbreak was attributed to Clade II of the virus, which is endemic in West Africa. That outbreak eventually was contained and the emergency ended in May 2023.
Yet, the virus has continued to spread and about a year ago, a new virus strain, known as Clade 1b, started spreading rapidly in the DRC and to neighboring countries. There have been over 15,600 cases in the DRC alone so far this year, with over 530 deaths. Clade 1b seems to be more virulent and more transmissible. It is spread through close physical contact with infected individuals. This means that sexual partners, household contacts, including children, are susceptible, as well as healthcare workers who are not properly protected.
Clade II of the virus also continues to spread, including recently reported 24 cases and three deaths in South Africa, where there are concerns around the virus impacting people who are HIV-positive.
The public health emergency of international concern declared in August 2024 was due to the alarming spread of Clade 1 in Central Africa, the lack of sufficient vaccine and antivirals in Africa, and the need for a coordinated global response to get the outbreak under control.
Why are there insufficient vaccines available if mpox has been around for a while?
Ensuring sufficient quantities of vaccine reach the most vulnerable populations in Africa is at the heart of this emergency. DRC has been doing its best to control the outbreak without access to vaccines and only started to receive a small number of doses. The affected countries must rely on donations from developed nations, as the cost is about $100 per dose. There are also complications getting vaccines to conflict-prone regions and ensuring the population is willing to accept the jab.
What is the risk factor of the disease spreading to the U.S.? Can it spread rapidly like COVID-19?
Unlike COVID-19, mpox requires close personal contact in order to spread between people. The virus can still spread to the U.S., as people travel around the world, but the risk to the general public from the virus circulating in the DRC right now is low. Those who are in close personal contact with people from affected countries or are healthcare workers are advised to take additional precautions, per the CDC.
Additionally, people in the U.S. who are impacted are fortunate to have access to both antivirals and vaccines.
Are there any lessons learned from the COVID-19 pandemic that are applicable to the containment of mpox? Are there any lessons you personally learned from your time as an advisor to the State Department and for President Biden’s COVID-19 task force that are applicable now?
Like in any outbreak, it is important to take early action and to devote resources for surveillance and response. Mpox is a reminder that there is still significant inequality around the world in terms of access to healthcare, access to medical countermeasures and support for infection, prevention and control. And outbreaks in insecure regions can fester and threaten large populations.
The field of pandemic preparedness and response suffers from a cycle of panic and neglect. After the declared ends of the COVID-19 pandemic and the 2022-2023 mpox health emergency, the world slipped into the ‘neglect’ phase of the cycle, which is one of the reasons we are now faced with the current mpox emergency.
What role does the global community and multilateral organizations like the World Health Organization have to curb the spread of mpox?
WHO is in charge of coordinating a global response to mpox, raising resources to support the response and ensuring that the populations that need drugs and vaccines are able to access them. They must also enhance surveillance and messaging so that there is situational awareness around how the virus is evolving and spreading so that impacted populations can take appropriate actions.
Are there any reasons why cases of mpox originate and are concentrated on the African continent?
Mpox is a zoonotic disease, which means it transmits from animals to humans. Animals that carry the virus, including Gambian rats and monkeys, are most often found in the tropical rainforests of Central and West Africa.
While the cases may originate in Africa, it is critical to have global vigilance. Animals carrying the virus have been exported in the past. In 2003, there were cases of the virus in the U.S. after direct contact with infected pets that had been exposed to exported animals from Africa.
Most importantly, the virus can then spread from human to human after initial spillovers from animals. This means that in our globalized world, people can carry the virus anywhere.